Like with mental illness, there are a lot of myths and misconceptions surrounding trauma disorders. Here’s a few answers to frequently asked questions (FAQs) and statements surrounding trauma disorders.
It’s a fad/new thing
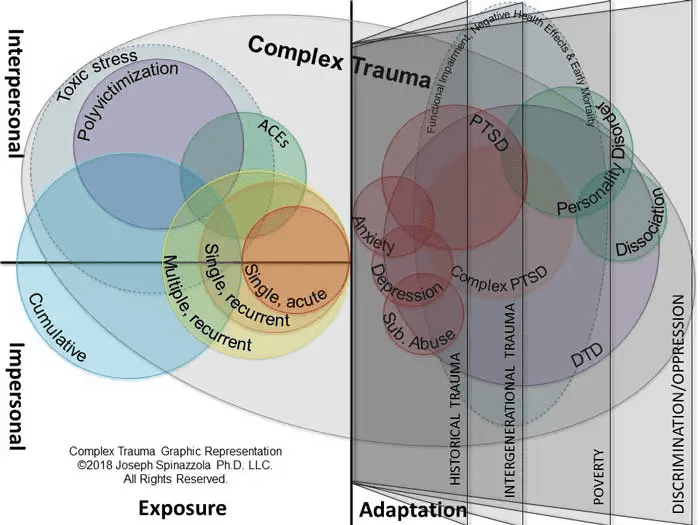
Trauma has been a part of the human condition for as long as there has been mankind. War, rape, incest, you name it, have been around for millennia. Writers such as Homer, Shakespeare and Dickens have written about the effects of trauma in their works. It’s not new. That PTSD wasn’t added to the DSM until 1980 doesn’t mean it didn’t exist before that. Formal attempts in medicine to define, diagnose and treat PTSD have been noted in American medicine since the 1760’s. That’s right – it took 220 years to add a disease that has been around since the dawn of time for mankind, to the ‘diagnosticians bible’ of mental disorders.
The same goes for disorders such as cPTSD. Just because the DSM hasn’t added it yet, doesn’t mean it doesn’t exist, that there hasn’t been extensive research done or isn’t enough proof of the condition. The World Health Organization has classified cPTSD in its International Statistical Classification of Diseases and Related Health Problems (ICD). That it’s not been added to the DSM isn’t because there isn’t enough knowledge about it, it’s because for 20 years they’ve been arguing about HOW to describe complex trauma.
You don’t get a trauma related disorder unless there’s some weakness in your personality
Wrong. Studies have shown that trauma in early stages of development affects the brain PHYSICALLY.
“Exposure to complex trauma in early childhood leads to structural and functional brain changes. Structural changes alter the volume or size of specific brain regions. Proven structural changes include enlargement of the amygdala, the alarm center of the brain, and shrinkage of the hippocampus, a brain area critical to remembering the story of what happened during a traumatic experience. Functional changes alter activity of certain brain regions. […] Many such abnormalities identified through neuroimaging that have previously been attributed to psychiatric illness have been scientifically proven to be the result of prior childhood maltreatment.”
Childhood maltreatment includes emotional abuse and neglect, and pretty much anything on the list of covert traumas.
If you don’t get what that means, let’s try an example.
You don’t tell someone with a proven brain disease, such as Alzheimer’s, to just get over themselves and act or think normally already. Yet this happens over, and over, and over again with people who suffer from trauma related disorders.
You don’t expect people with a physical disability to just grow a limb back, or get up and walk already. Well, unless you’re just that much of an asshole I suppose.
No. You allow them to do as much as they possibly can autonomously, and help them when they ask for it, or if they’ve reached their limits.
Trauma related disorders only affect thinking, behavior or the brain
No. The changes in the brain due to trauma during certain stages of development may affect people physically. These changes can lead to an “overproduction of stress hormones in childhood that can wear down the immune system and lead to depletion by adulthood of hormones necessary tolerate and recover from stressful situations encountered in daily life.”
That’s right: it can lead to the wearing down of the immune system, well into adulthood, which is “a complex network of organs, cells and proteins that defends the body against infection, whilst protecting the body’s own cells.”
If it’s a question of a brain disease, you can’t do anything to change or improve
Trauma disorders stem from childhood
Myth. People who are perfectly capable of dealing with trauma in a healthy manner may develop a trauma disorder if they suddenly face a number of traumas in rapid succession.
People who suffer from trauma disorders can’t handle stress or crisis
Myth. People who suffer from trauma disorders may deal with an acute, stand alone trauma, stressors or crisis, incredibly well. Most likely because they’ve been managing their disease, with or without help, effectively, and in a lot of cases undetected, for years.
In order to survive, these people have found a range of ways to deal with stressors or crisis. And some of these survival mechanisms actually make them much more capable of taking over during crisis, and much less likely to fold under pressure in their jobs, social situation or relationships when they are free from personal triggers.
Trauma disorders can’t stand alone, there’s always a co-morbid other psychiatric condition
A lot of trauma disorders, especially those pertaining to complex trauma, are misdiagnosed as other conditions. The problem is that complex trauma may lay at the root of other mental illnesses as well, causing overlap. Often, either because mental health professionals are not informed about trauma, let stand complex trauma, or they do not look beyond the DSM, people suffering from trauma disorders initially get diagnosed with the more well-know and often partially overlapping disorders. Personality disorders, anxiety disorders, dissociative disorders, etc.
Although this is not an uncommon occurrence, it does create a huge problem for patients suffering from cPTSD. It’s immensely frustrating to be asked to change your thinking or behavior or feelings, to follow one therapy after the other that should work for the individual disorders, and then don’t.
It means that in general, standard protocols treat symptoms first, and keep treating the symptoms, not the underlying trauma(s). In some cases the treatments actually worsen the underlying trauma. But then the downward spiral starts again – because the worsening of the condition is seen as a personality disorder, and another diagnosis is added to make the whole thing ‘fit’ according to standards that are years behind the facts.
How we treat people with trauma related disorders has no bearing on their ability to cope
That’s absolutely not true. When people with trauma related mental illnesses are asked “what’s happened to you” instead of being “asked” “what’s wrong with you”, it can lead to self-actualization.
Whatever is “wrong” with them is a survival mechanism. They adapted to overwhelming situations in order to survive. That requires strength, adaptivity, self-reliance, and quite a bit of out-of-the-box thinking. In some cases an enormous amount of strength, adaptivity, self-reliance and out-of-the-box thinking.
That they are incapable, without help, of turning off those mechanisms, is not a sign of weakness. The world is still unsafe to them, regardless if the acute or chronic trauma(s) that caused the development of the survival mechanism is no longer an active threat in the here and now.
How do you diagnose cPTSD?
I was literally asked this by a psychiatrist a few days ago. If I ever find the answer, I’ll get back to you. But as it’s taken centuries for medical professionals to formulate the definition of PTSD, which is usually related to one acute trauma, well enough for it to be added to the DSM.
I doubt I’ll be able to answer this question anytime soon.
How to diagnose cPTSD has been answered by the WHO, but they’re not seen as the bible of diagnostics when it comes to mental illness.
Currently it seems that, unless a diagnostician is:
- actually aware of, and has researched, the differences between acute, chronic and complex trauma;
- is aware of its effects on mental health in general, and its effect when it comes to mental illness specifically.
the diagnosticians first throw whatever disorder fits best in their opinion at that time, keep adding extra disorders to fit symptoms that don’t fit the initial diagnosis, and then, when all else fails, add cPTSD as a possible co-morbid condition.
I wonder what would happen if the traumas were dealt with before even attempting to diagnose, let stand treat, a plethora of disorders whose base assumptions are all “there is something wrong with you” when it’s been a question of how do we help you deal with what’s happened to you, and teach you how to manage whatever survival skills you’ve taught yourself that may not be helpful in all situations anymore.