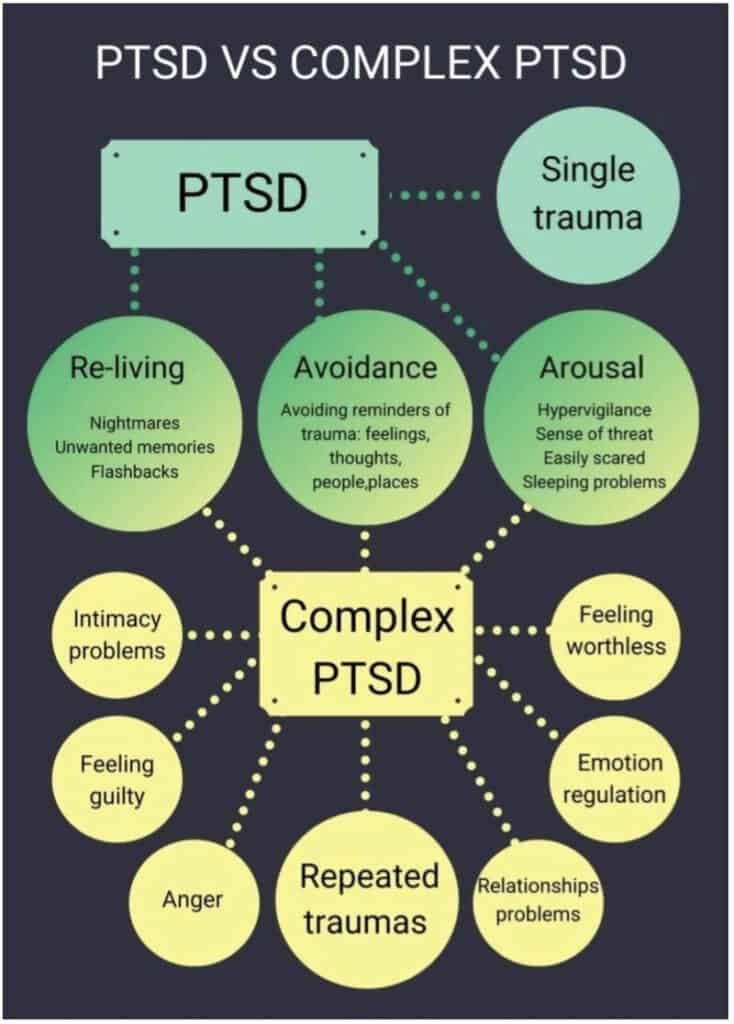
cPTSD or Complex Post Traumatic Stress Disorder is a recognized disorder, despite not being defined for the DSM-5 yet. The World Health Organization does though. According to the International Classification of Diseases (ICD-11) cPTSD is defined as follows:
“Complex post traumatic stress disorder (Complex PTSD) is a disorder that may develop following exposure to an event or series of events of an extremely threatening or horrific nature, most commonly prolonged or repetitive events from which escape is difficult or impossible (e.g. torture, slavery, genocide campaigns, prolonged domestic violence, repeated childhood sexual or physical abuse). All diagnostic requirements for PTSD are met. In addition, Complex PTSD is characterized by severe and persistent
1) problems in affect regulation;
2) beliefs about oneself as diminished, defeated or worthless, accompanied by feelings of shame, guilt or failure related to the traumatic event; and
3) difficulties in sustaining relationships and in feeling close to others.
These symptoms cause significant impairment in personal, family, social, educational, occupational or other important areas of functioning.”
To put it simply:
IF you have PTSD
AND have a lot of problems functioning in difficult situations.
PLUS you feel less than you used to, defeated or worthless, as well as ashamed, guilty or like a failure because of a traumatic event.
AND you have trouble keeping up your relationship and feeling close to others.
PLUS these things are causing trouble in your personal life, with your family, your friends, your schooling, work or other important areas of function
AFTER you were exposed to a traumatic event, or series of events,
- that were horrific or threatening in nature and
- usually took place over a long time and repeated themselves
- from which escape was difficult or impossible
It might be cPTSD
You might also experience:
- Suicidal thoughts or tendencies
- Substance abuse
- depressive symptoms
- psychotic symptoms
- somatic complaints
Symptoms
These are some of the symptoms of complex post traumatic stress disorder
- Deep fear of trust
- Muscle armoring
- Trouble regulating emotions
- Emotional flashbacks
- Hyper-vigilance about people
- Disassociation
- Persistent sadness
- Feeling suicidal
- Loss of faith
- Terminal feeling of being alone
- Profoundly hurt inner child
- Helplessness
- Toxic Shame
- Repeated search for a rescuer
About defining complex trauma and cPTSD
This article will be updated with further research and sources soon.
Sources
DEVELOPING THE COVERT TRAUMATIC EXPERIENCE SCALE (COTES): A RETROSPECTIVE EARLY PSYCHOSOCIAL TRAUMA ASSESSMENT TOOL
Tiffany E. Vastardis PhD, LMHC, CCTP, CMHIMP
Clinical Education Specialist • Florida Residential Clinical Training Liaison • Mental Health Researcher • Licensed Psychotherapist • Clinical Trauma Specialist • Integrative Medicine Practitioner
Factors contributing to the onset of cPTSD
Eight contributing factors to the expression of cPTSD symptomology have been
identified: 1) intensity, duration, and timing, 2) genetics, 3) environment, 4) in-utero
environment, 5) family dynamics, 6) modeling, 7) presence of a developmental and/or
learning disorder, and 8) lack of resilience factors (Schwartz, 2016).
Intensity, duration, and timing
The longer the duration and the greater the intensity of the trauma, the more likely
one is to develop a traumatic response. Timing also matters, as children tend to be the
most susceptible to the impact of such events, due to their fragile neurodevelopmental
status. In addition, adolescents are also highly susceptible, due to threats to identity
development (Schwartz, 2016).
Genetics
Expressions of trauma-related anxiety responses may have a genetic link, where
having a parent who suffers from a trauma-related disorder lends to a higher risk for the
development of the trauma-related responses evident in trauma disorders, due to inherited
abnormalities in the wiring of neurocircuitry (Schwartz, 2016).
Environment
Parents with trauma-related disorders may treat their children differently than
those of whom experienced healthy development. As a result, greater disruptions in care
may affect the children of traumatized parents, leading to feelings of intrusion, ostracism,
and abandonment. Hence, children may respond in fear or anger, lending to a
perpetuation of environmental cycles of abuse, where the parent reacts to the child’s fear
responses via violence, aggression, and/or neglect (Schwartz, 2016).
In-utero environment
Infants born to mothers who were exposed to traumatic events while pregnant
evidence lower birth rates and faulty production of cortisol. As a result, these infants may
be more difficult to soothe during infancy, lending to disrupted attachment, colic, and
hypervigilance during childhood. These factors make an individual inherently susceptible
to a higher proclivity of developing pathological responses in the face of trauma
(Schwartz, 2016).
Family dynamics
Dysfunctional comfort levels with a child’s gender, readiness to raise a child,
and/or events surrounding a child’s birth may affect parental treatment styles. In the event
of unplanned pregnancies, resentment may lend to projection of disillusionment upon the
child. Furthermore, a traumatic birthing experience may lead to a misappropriation of
blame towards the child, resulting in maltreatment and/or abuse (Schwartz, 2016).
Modeling
Children who were raised in abusive households are, most often, exposed to
multiple risk factors. Such factors include: inconsistent medical care, insufficient
modeling of self-care and coping behaviors, lack of support, and both physical and
proximal neglect. These adverse experiences are traumatic, in-and-of-themselves.
Furthermore, such outcomes of abuse may lead to further traumatization, especially that
of which is psychosocial, across various other contexts of life. Finally, modeling of
dysfunctional behaviors, such as substance abuse and promiscuity, can prime children for
traumatic exposure across the lifespan. Furthermore, children who have experienced such circumstances are more likely to replicate similar behaviors as adults, reinforcing
generational cycles of abuse (Schwartz, 2016).
Presence of a developmental and/or learning disorder
Research indicates strong correlations between developmental disorders, such as
ADHD, and child abuse. Here, faulty coping and a lack of patience on behalf of the
parents regarding cognitive differences, hyperactivity, and impulsivity in affected
children may both precipitate and perpetuate patterns of abuse. These correlations are
bidirectional, as children who are abused are also more likely to develop learning
disorders and other maladaptive expressions of functioning and behavior (Schwartz,
2016).
Lack of resilience factors
Protective resources alleviate the impact of childhood trauma. A child’s primary
protective resource is his and/or her caretakers. When parents fail to adequately support
their children, they are left subject to traumatic exposure, taking place both inside and
outside of the household. Additional protective factors include: a safe community
environment, engagement in prosocial activities, and positive peer relations, all of which
can serve to build resilience in youth. Lack of such resilience factors can lend to faulty
attachment, amplified feelings of neglect and alienation, and an inability to trust the world surrounding the developing child. These patterns of behavior and perception can be carried into adulthood (Schwartz, 2016).
cPTSD and Treatment
Psychological interventions for ICD-11 Complex PTSD symptoms: Systematic review and meta-analysis